World leaders are expected to meet at the 79th United Nations High-Level Meeting on Antimicrobial Resistance (AMR) on 26 September 2024. This is the second time historically that such a UN High-Level Meeting (UNHLM) on AMR is being organized (first UNHLM on AMR was held in 2016).
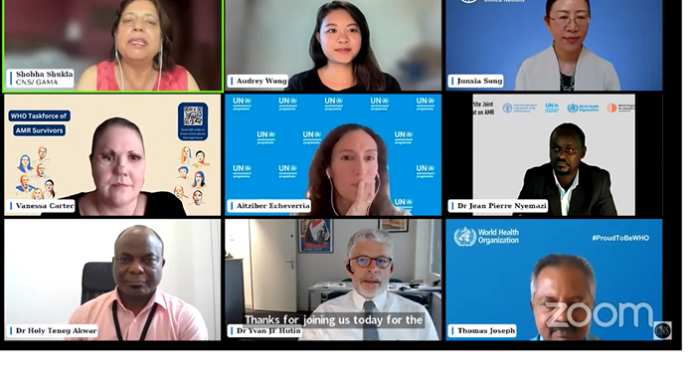
“1st UNHLM on AMR in 2016 was a milestone and drove much of the key results that we can see today in AMR response. Quadripartite organizations too united to address AMR using One Health approach worldwide (these include: the Food and Agriculture Organization of the United Nations – FAO, United Nations Environment Program – UNEP, World Health Organization – WHO, and World Organization for Animal Health – WOAH). Joint strategic framework of the 4 quadripartite organizations (FAO, UNEP, WHO and WOAH) defines and guides our joint-collaboration, global coordination and cooperation in addressing AMR,” said Dr Jean Pierre Nyemazi, acting director, Global Coordination and Partnership Department, and director of Quadripartite Joint Secretariat on Antimicrobial Resistance (AMR), WHO.
The theme of 2nd UNHLM on AMR on 26 September 2024 is, “Investing in the present and securing our future together: Accelerating multisectoral global, regional and national actions to address antimicrobial resistance.”
“Final draft text of the political declaration which has been submitted to all the heads of governments worldwide and which will be the basis of all discussions at the global meet on 26th September at UNHLM on AMR is online now” said Dr Nyemazi.
Drug-resistant infections know no borders, meaning no single country can respond to AMR alone. UNHLM on AMR meeting is an important opportunity for world leaders to collectively address the looming threat AMR poses to global health, food security, and achieving the 2030 Sustainable Development Goals (SDGs).
Urgency to prevent AMR if we are to deliver on heath for all and SDGs
“Antimicrobial resistance (AMR) is currently one of the greatest global threats. It results in millions of deaths, long-lasting disabilities and increased health care costs. It also has severe impacts on livelihoods, threatens food security and results in loss of animal lives,” said Dr Nyemazi.
“In 2019, 4.95 million deaths were associated with drug-resistant bacterial infections, including 1.27 million deaths directly attributable to bacterial antimicrobial resistance, 20% of whom were children under 5. Without a stronger response to prevent AMR, there will be an estimated average loss of life expectancy of 1.8 years globally by 2035. Globally AMR could result in US$ 1 trillion of additional healthcare costs per year by 2050 and US$ 1 trillion to 3.4 trillion of gross domestic product losses per year by 2030. Treating drug-resistant bacterial infections alone could cost up to US$ 412 billion annually, coupled with workforce participation and productivity losses of US$ 443 billion,” added Dr Nyemazi.
Primary driver of AMR is the misuse and overuse of antimicrobials (antibiotics, antivirals, antifungals, antiparasitics) in human, animal and plant health. It is further complicated by increased incidence of infections due to the poor quality of drinking water, low access to sanitation and insufficient infection control in healthcare facilities. Inappropriate disposal of waste, especially those with antimicrobials, contributes to the spread of AMR.
“Rising levels of AMR will hinder progress towards many of the Sustainable Development Goals (SDGs), particularly those focusing on health and well-being, poverty reduction, food security, environment and economic growth,” said Dr Nyemazi.
AMR and food systems
Since antimicrobials are used in multiple sectors, and it is often disseminated through the environment, the impact of AMR is felt in all the sectors they are used and beyond. Therefore, a One-Health approach which recognizes that the health of animals, humans, plants and the environment are interlinked, is essential to prevent and respond to AMR.
“AMR is a very complex crisis that impacts every aspect of our lives especially within the food system. The misuse of essential drugs in food production, livestock farming, aquaculture, or crop production, accelerates the emergence and spread of resistance strains. These resistant strains of disease-causing microbes can transfer from animals to humans through direct contact or through the agriculture-environment or the food chain, worsening the AMR crisis. This also has significant implications for food safety, food security and economic wellbeing of millions of farming households. Common bacterial infections are becoming harder -and sometimes impossible – to treat,” said Dr Junxia Song, senior animal health pfficer, Food and Agriculture Organization of the United Nations (FAO).
“AMR threatens livelihoods of 1.3 billion people who depend on livestock. The World Bank projects that in high AMR impact scenario, livestock production in low-income countries could decline by 11% by 2050. AMR is raising costs for farmers and driving up food prices. One of the major challenges in addressing AMR in aquatic-food system is the limited funding available,” added Dr Junxia Song. “We must promote responsible use of antimicrobial medicines in agriculture and food systems alongside promoting best practices at farm level to reduce reliance on medicines.”
AMR is faceless but those who suffer (humans, animals, plants) are not
“AMR is faceless often when it affects or contribute to the mortality of an animal or a person (or plant). The underlying disease gets the blame and AMR may go unnoticed. So, most of the AMR estimates we see could be underestimates,” said Dr Holy Teneg Akwar, deputy head of the Antimicrobial Resistance and Veterinary Products Department, World Organization for Animal Health (WOAH).
The WOAH Report on antimicrobial agents intended for use in animals 2024 has not only analyses of 2021 antimicrobial quantities but also trends from 2019-2021 (81 countries). Veterinary monitoring and surveillance system for substandard and falsified veterinary medicinal products – had 62 member countries – largest from Africa (34.5%), then Asia Pacific (23.6%), Americas (21.8%), Europe 14.5%), and Middle East (5.4%).
“We have to enhance access to high-quality vaccines along with good animal husbandry practices, biosecurity, diagnostic tools, and develop alternatives to antimicrobials. Governments should aim at having defined animal vaccination strategies according to WOAH’s priority list of diseases where vaccines could reduce the use of antimicrobials, with a funded implementation plan by 2030,” added Dr Holy Teneg Akwar.
AMR and the environment
“The environment plays a key role in development, transmission and spread of AMR. Tackling AMR requires a multisectoral One Health approach that considers the health of humans, animals, plants, and the wider environment, including ecosystems as interconnected and interdependent,” said Aitziber Echeverria, AMR coordinator, chemicals and health branch, industry and economy division, UN Environment Program (UNEP).
“Three economic sectors and their value chains are potential drivers of AMR development and spread: 1) Pharmaceuticals and other chemical manufacturing; 2) Agriculture and food production; 3) Healthcare systems -and also municipal systems (waste and wastewater). We have to enhance environmental governance, planning and regulatory frameworks, generate evidence and knowledge to inform policy (to improve reporting, surveillance and monitoring, research) and raise awareness. We must also scale up preventative actions, with private sector engagement, addressing key value chains affecting AMR in the environment,” added Aitziber Echeverria.
“As new antibiotics were discovered, it is important to note that how fast resistance was reported soon after their discovery. For instance, Sulfonamides were discovered in 1930s and within 10 years, there were Sulfonamide-resistant microbes. In 1940s, penicillin was discovered, and resistance was reported in next few years. Research pipeline for new antimicrobials is drying up. That is why we need stronger commitments at the UNHLM on AMR to save our medicines,” said Dr Yvan JF Hutin, director, Department of Control, Surveillance and Prevention of Antimicrobial Resistance, World Health Organization (WHO).
“One of the key elements to prevent AMR is a people-centred public health approach. Primary healthcare to advance universal health coverage needs to be at the heart of our approach. Timely and accurate diagnosis is key so that the person can be offered quality assured treatment,” said Dr Hutin.
“World leaders need to fully finance the AMR response. Effective governance, investing in AMR prevention while we accelerate research and development, and addressing issues of inequitable access to diagnostics and antimicrobial medicines must be prioritised. What the world needs now are bold, transformational, and firm commitments from the heads of states, which will ensure that the implementation of action plans on AMR are accelerated and effective. There is no time to waste, we must act together to preserve the effectiveness of these global public goods to ensure a safe planet for our children,” said Dr Nyemazi.
“Patient stories are crucial and should be acknowledged in how we communicate, shape policies, foster innovation, improve medical education, and implement strategies to address Antimicrobial Resistance (AMR), including improving access to quality-assured treatments, diagnostics and enhancing Water, Sanitation, and Hygiene (WASH) in low- and middle-income countries. As a South African patient, these issues, and more, are highly concerning as well as awareness raising around AMR,” said Vanessa Carter, AMR survivor, Chairperson of WHO Task Force of AMR Survivors, and Founder Leader of The AMR Narrative.
“We as young people are concerned on how our future looks like with growing (and preventable) global health threats like AMR. As a young pharmacist, I see cases with young patients too who develop AMR, and it is very heartbreaking,” said Audrey Wong, Chairperson, Quadripartite Working Group on Youth Engagement for AMR.