With simple to treat infections increasingly becoming difficult to treat (or even incurable) due to drug resistance, global health, as well as food safety and security are facing acute threats. Misuse and overuse of antimicrobial medicines are making bacteria, virus, fungi or parasites drug-resistant and causing antimicrobial resistance (AMR).
The misuse and overuse of antimicrobial drugs in human health, animal health and livestock, food and agriculture are fuelling antimicrobial resistance (AMR). Additionally, environmental pollution – such as untreated hospital and community wastewater, pharmaceutical effluents, and agricultural run-off – plays a growing role in enabling resistant pathogens to emerge and persist across sectors. The consequences of AMR are far-reaching, affecting human and animal health, food safety and security, and placing additional strains on healthcare systems and economies.
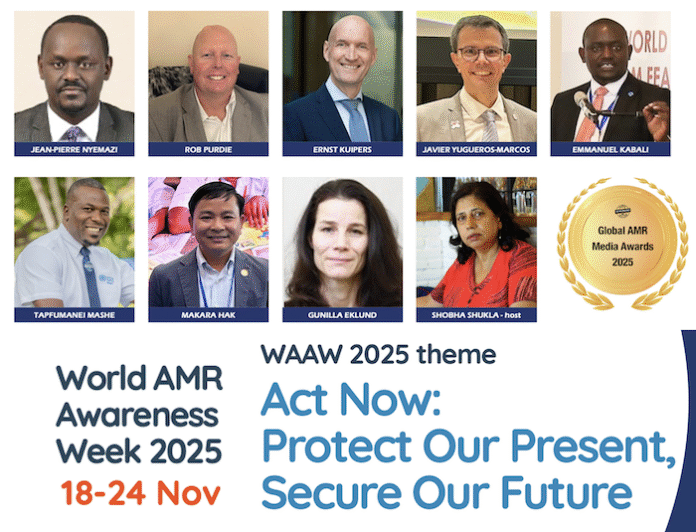
Addressing AMR requires urgent, coordinated action and sustained commitment from governments and diverse sectors across the One Health spectrum, said Dr Jean-Pierre Nyemazi, Director of the Quadripartite Joint Secretariat on AMR. The Quadripartite Joint Secretariat has brought 4 global agencies on human health (WHO), food and agriculture (FAO), environment (UNEP) and animal health (WOAH) together to address AMR using the One Health approach.
Two lives lost every minute due to AMR
“Today, one out of every six bacterial infections confirmed in the laboratory is resistant to antibiotics,” said Dr Javier Yugueros-Marcos, head of the Antimicrobial Resistance & Veterinary Products Department, World Organization for Animal Health (WOAH).
AMR is already linked to nearly five million deaths each year, including 1.14 million deaths directly caused by bacterial AMR. “That is two lives lost every minute. Since 2016, countries have worked hard to prevent AMR. Over 90% of the countries (178 countries) have national AMR action plans. But only 22% are fully implementing the national AMR action plans with monitoring and financing in place. So, that is why world leaders stepped up last year in 2024 with another bold commitment enshrined in the Political Declaration adopted in the UNGA 2024 High Level Meeting: 60% of countries must have fully funded national AMR action plans and implement them,” said Dr Nyemazi.
“For us to reach that goal, governments also committed to mobilise at least US$ 100 million by 2030, including through AMR Multi-Partner Trust Fund (AMR MPTF) and other mechanisms. This is a powerful signal that the world understands the urgency and shared responsibility. However, technical solutions alone won’t win this fight. We need a shared responsibility,” said Dr Nyemazi.
Fully replenish AMR MPTF
Till 2019 there was no dedicated funding mechanism to support governments address AMR with One Health inter-sectoral approach. That is why in 2019, an Antimicrobial Resistance Multi-Partner Trust Fund (AMR MPTF) was setup under the United Nations. AMR MPTF is the world’s principal pooled-financing mechanism specifically to support low- and middle-income countries implement and strengthen multisectoral AMR National Action Plans.
World AMR Awareness Week (WAAW 2025) observed globally every year during 18-24 November is another reminder for richer governments to fully replenish the fund for global health security.
“The gains made in AMR policy development risk stalling without the means to act,” said Dr Emmanuel Kabali, AMR Project Coordinator, Food and Agriculture Organization of the UN (FAO).
The AMR MPTF uniquely harnesses the expertise of the AMR Quadripartite agencies to advance country-led actions across human, animal, plant, and environmental sectors. It is breaking silos because it blends high-level global governance, surveillance, and policy with collaborative local action by leveraging knowledge and coordinating efforts of resource partners, governments, community-based organisations, and other sectors. AMR MPTF is bridging and filling gaps.
AMR MPTF saving lives and reducing economic loss in Zimbabwe
Thanks to AMR MPTF, Zimbabwe revived domestic production of the BOLVAC vaccine to combat tick-borne disease (in cattle etc), reducing antibiotic misuse and linking the AMR response to high-priority livestock sector issues, ensuring sustainability, said Dr Tapfumanei Mashe, AMR Project Coordinator, WHO Zimbabwe. “Zimbabwe is an agricultural economy. So, with initiatives like BOLVAC vaccine we are not merely addressing antimicrobial resistance but also addressing the economic loss it was causing.”
“There are a lot of scientific studies to show impact of expanded vaccination programmes and improved water, sanitation and hygiene in addressing AMR effectively – we can avert 750,000 deaths occurring due to AMR every year in low- and middle-income countries (LMICs) with such proven approaches,” said Dr Mashe.
“In 2019, Zimbabwe also introduced typhoid conjugate vaccine (TCV) to prevent typhoid fever caused by bacteria Salmonella typhi. Typhoid fever was also a cause of increasing AMR. Using AMR MPTF resources we are tracking impact of introducing TCV. We saw a reduction in incidence of typhoid fever from 1373 per 100,000 before introduction of TCV vaccine to 341 per 100,000 after the introduction of TCV vaccine. This has also resulted in reduction of AMR,” said Dr Mashe.
“By introducing typhoid conjugate vaccine, we are not merely addressing AMR but also addressing healthcare of the people and reducing costs government was incurring for those with typhoid. In 2018, first-line medicine for typhoid (ciprofloxacin) was not working because of drug resistance, so we had to treat with azithromycin which was more expensive. So, typhoid conjugate vaccine has not only reduced AMR but also reduced the expenditure for government as well mortality and morbidity for the people,” said Dr Mashe.
“As a result of multi-sectoral team working together, we have strengthened surveillance, where we are tracking antimicrobial resistance in different sectors, including human health, animal health, environment and food and agriculture. Quality of medicine is another important area to focus on for us in Zimbabwe. Thanks to AMR MPTF, Zimbabwe is also tracking phosphide resistance by setting up a surveillance system where we can check the prevalence of fortified medicines circulating in the country,” added Dr Mashe.
Cambodia had ambition but no means: MPTF enabled it to go One Health way
In 2019, Cambodia had a multi-sectoral national AMR action plan but hardly any finances to implement it. AMR MPTF funding not only enabled it to implement the plan but also transition from AMR inter-ministerial committee towards a broader One Health governance framework.
“Without enough financial resources, before MPTF funding, Cambodia’s efforts to implement AMR National Action Plan were very fragmented. When MPTF funding came to Cambodia, we were able to significantly step up the implementation of Cambodia’s National Action Plan on AMR. Resourced by MPTF, we established Cambodia’s national multi-sectoral coordination body based on the One Health approach. It brought together different agencies in sectors like human health, animal health and livestock, food and agriculture, and environment,” said Dr Makara Hak, Adviser on Animal Health, FAO (Food and Agriculture Organization of the United Nations), Cambodia. “Thanks to MPTF support, different committee meetings were convened regularly to review policy regulations to guide implementation of Cambodia’s AMR National Action Plan – something which could never happen in the past.”
“Cambodia could also accelerate its capacity building efforts at national as well as sub-national levels to address AMR. Over 200 provincial and district veterinarians and over 1000 village animal health workers in private sector have been trained as per the AMR treatment guidelines. All this could happen due to the support of MPTF,” confirmed Dr Mak.
“Thanks to MPTF, Cambodia could invest in strengthening animal health laboratories which is very important for addressing AMR as well as for AMR surveillance systems. Cambodia introduced Laboratory Information Management System to ensure that data meets international standards. We also invested in building the capacity of the academia and laboratories (including fishery laboratories) as part of Animal Health Laboratory Network,” said Dr Mak.
“This progress in Cambodia has unlocked new opportunities to further strengthen AMR response. We received US$ 1 million from AMR MPTF to strengthen Cambodia’s capacity which enabled us to secure another US$ 34 million for AMR and One Health in Cambodia through German Development Bank (KfW). Now, we can not only sustain these efforts but also further build upon them,” he said.
Cambodia recently endorsed the 2nd phase of AMR multi-sectoral action plan 2025-2030. We are going to develop additional legally binding policy document to strengthen and reinforce antimicrobial use in animal health sector,” added Dr Mak.
“AMR is invisible, I am not” says Rob Purdie, AMR survivor.
“One of the best ways to humanize the difficult issue of AMR is by using lived experiences,” said Rob Purdie, AMR survivor and member of WHO Task Force of AMR Survivors.
“AMR remains one of the most serious and complex health and developmental challenges of our time. It threatens not only modern medicine but also the very foundations of global health security, food safety and sustainable development. Nearly every country now has a national AMR action plan, but only 11% of them have allocated the necessary funding for implementation,” said Professor Ernst Kuipers, Global Leaders Group on AMR (GLG) member, and Former Minister of Health, Welfare and Sport, Netherlands.
“Through the AMR multi-partner trust fund, low- and middle-income countries are building surveillance systems, strengthening laboratory capacity, improving infection prevention and control, and promoting responsible use of antimicrobials in human, animal and plant health. These initiatives are not abstract. They save lives. They protect livelihoods and they safeguard medicines we depend on,” said Prof Kuipers.
“If we act decisively now, we can preserve the effectiveness of lifesaving medicines for generations to come. If we however delay, we risk losing the very tools that make modern healthcare possible,” concluded Prof Kuipers.
Investing in AMR MPTF is smart
“The European Commission supports and invests in the AMR MPTF because it ensures donor coordination. It avoids duplication and fragmentation, and it gives the beneficiary countries the flexibility to focus on their priorities and their needs. And it also strengthens the One Health response by aligning all the relevant sectors,” said Dr Gunilla Eklund, the European Commission’s Directorate-General for Health & Food Safety (DG SANTE), European Commission.
“MPTF is more than just a fund. It’s a platform for partnership. And as such, we believe it’s a smarter model for aid. It allows collective action to deliver more than what isolated projects would have done by themselves. And in these times, I think we cannot emphasize enough the importance of pooling resources in the current climate of tight budgets. The MPTF is a tried and a trusted mechanism that is efficient and effective. It ensures that the investments align, with the country needs and the country’s own priorities,” added Dr Eklund.